Counseling to Patients with HPV Infection
The following key counseling messages should be conveyed to all patients diagnosed with HPV infection:
- Genital HPV infection is very common. Many types of HPV are passed on through genital contact, most often during vaginal and anal sexual contact. HPV can also be spread by oral sexual contact.
- Most sexually active adults will get HPV at some point in their lives, though most will never know it because HPV infection usually has no signs or symptoms.
- In most cases, HPV infection clears spontaneously, without causing any health problems. Nevertheless, some infections do progress to genital warts, precancers, and cancers.
- The types of HPV that cause genital warts are different from the types that can cause anogenital cancers.
- Within an ongoing sexual relationship, both partners are usually infected at the time one person is diagnosed with HPV infection, even though signs of infection might not be apparent.
- A diagnosis of HPV in one sex partner is not indicative of sexual infidelity in the other partner.
- Treatments are available for the conditions caused by HPV (e.g., genital warts), but not for the virus itself.
- HPV does not affect a woman’s fertility or ability to carry a pregnancy to term.
- Correct and consistent male condom use might lower the chances of giving or getting genital HPV, but such use is not fully protective, because HPV can infect areas that are not covered by a condom.
- Sexually active persons can lower their chances of getting HPV by limiting their number of partners. However, HPV is common and often goes unrecognized; persons with only one lifetime sex partner can have the infection. For this reason, the only definitive method to avoid giving and getting HPV infection and genital warts is to abstain from sexual activity.
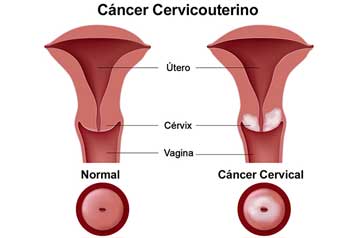
- Tests for HPV are now available to help providers screen for cervical cancer in certain women. These tests are not useful for screening adolescent females for cervical cancer, nor are they useful for screening for other HPV-related cancers or genital warts in men or women. HPV tests should not be used to screen:
- men;
- partners of women with HPV;
- adolescent females; or
- for health conditions other than cervical cancer.
Anuncios - Two HPV vaccines are available, both of which offer protection against the HPV types that cause 70% of cervical cancers (i.e., types 16 and 18); the quadrivalent vaccine (Gardasil) also protects against the types that cause 90% of genital warts (i.e., types 6 and 11). These vaccines are most effective when all doses are administered before sexual contact. Either vaccine is recommended for 11- and 12-year-old girls and for females aged 13–26 years who did not receive or complete the vaccine series when they were younger. The quadrivalent HPV vaccine can be used in males aged 9–26 years to prevent genital warts.
The following are specific counseling messages for those persons diagnosed with genital warts and their partners:
- Genital warts are not life threatening. If left untreated, genital warts might go away, stay the same, or grow in size or number. Except in very rare and unusual cases, genital warts will not turn into cancer.
- It is difficult to determine how or when a person became infected with HPV; genital warts can be transmitted to others even when no visible signs of warts are present, even after warts are treated.
- It is not known how long a person remains contagious after warts are treated. It is also unclear whether informing subsequent sex partners about a past diagnosis of genital warts is beneficial to the health of those partners.
- Genital warts commonly recur after treatment, especially in the first 3 months.
- Women should get regular Pap tests as recommended, regardless of vaccination or genital wart history. Women with genital warts do not need to get Pap tests more often than recommended.
- HPV testing is unnecessary in sexual partners of persons with genital warts.
- If one sex partner has genital warts, both sex partners benefit from getting screened for other STDs.
- Persons with genital warts should inform current sex partner(s) because the warts can be transmitted to other partners. In addition, they should refrain from sexual activity until the warts are gone or removed.
- Correct and consistent male condom use can lower the chances of giving or getting genital warts, but such use is not fully protective because HPV can infect areas that are not covered by a condom.
- The Gardasil vaccine, which has been approved for use in males and females aged 9–26 years, protects against the HPV types that cause 90% of genital warts (i.e., types 6 and 11).